Solutions
The MaxWell Brain MAP – Your Memory Loss Solution
5.7 million U.S. adults have Alzheimer’s disease. Many more have early stages of decline. With Personalized Systems Medicine® from MaxWell Brain, there’s a better path to prevent cognitive decline, improve function, and maintain independence.
The MaxWell Brain MAP is designed to identify and simultaneously address the underlying causes of cognitive decline, specifically tailored to each individual patient. It enables personalized care for outcomes that make a difference.
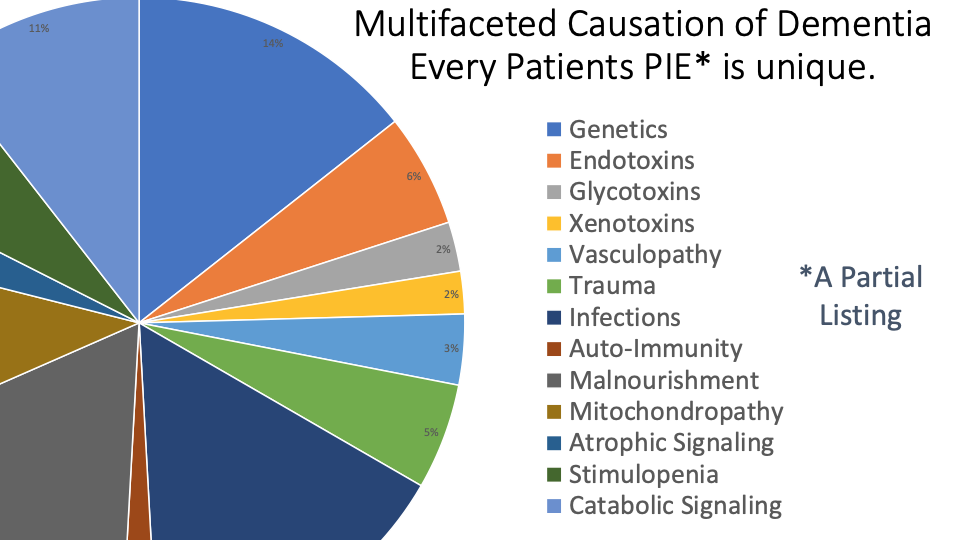
Multiple Contributors
There are multiple underlying causes of memory loss and Alzheimer’s disease. Each patient presents a different set of contributors calling for a different combination of interventions.
Our Process
The MaxWell Brain MAP is designed for patients with mild cognitive impairment, mild dementia, mild Alzheimer’s disease, or for those desiring to prevent such diagnoses ever occurring. Our service analyzes patient medical data to create personalized care plans. The care plans consist of recommendations of FDA-approved medications, nutraceuticals, and lifestyle improvements.
Personalized Systems Medicine® Engine
Our precision medicine engine uses artificial intelligence to process big data on patients. It applies medical knowledge to recommend evidence-based and highly-personalized treatment paths.
Care Plan Creation
We provide two versions of the personalized care plan – one for the physician and a simplified version for the patient. The physician prescribes the care plan as appropriate and reviews it with the patient.
Update Care Plan, Repeat
Patients are periodically retested at the request of the physician and their care plan is updated every six months.
Every 65 seconds, someone in the United States develops Alzheimer’s disease.
Yet, over 300 drugs for Alzheimer’s disease have failed in the FDA process over the last 20 years. It is clear that individual drugs don’t work.
Well, what does work then? Multiple studies have demonstrated that personalized combination therapy approaches have great potential in improving outcomes. With precision medicine from MaxWell Brain, there’s an opportunity to advance care for afflicted individuals.
Early Identification. Combination Therapy. Lasting Patient Benefits.
The MaxWell Brain MAP is based on many large studies such as the FINGER study, and delivers measurable clinical results.
The MaxWell Brain MAP – Clinical Results
Patient percentages with steady or improved cognitive status following implementation of The MaxWell Brain MAP.

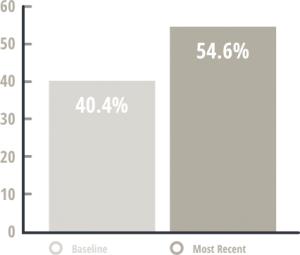
The numbers don’t lie.
2.8
Participants received an average of 2.8 personalized care plans over 8.4 months.
76%
76% of the studied population improved or held steady on repeated CNS-VS composite memory scores, with overall scores improving from 40.4% (below average) to 55.9% (slightly above average).
57%
57% of the MCI subset participants demonstrated improvement or held steady in their CNS- VS composite memory scores.
Source:
Walker, J Q.; Keine, D; Sabbagh, M. “DEVELOPMENT, APPLICATION, AND RESULTS FROM A CLINICAL INFORMATICS PLATFORM THAT ENABLES A MULTI-MODAL TREATMENT PROTOCOL FOR ALZHEIMER’S DISEASE (AD).” The Journal of Alzheimer’s and Dementia, 2017.
The FINGER Study: The Lancet, 2015.
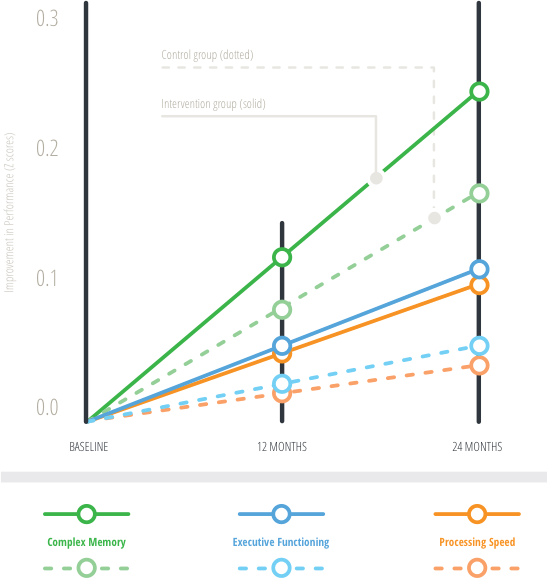
A two-year multi-domain intervention trial followed a personalized treatment comprising dietary changes, exercise, cognitive training, and vascular risk monitoring.
The intervention group scored 25% higher on neuropsychological tests than the control group.
Executive functioning and processing speed were also higher in the intervention group versus the control group, with the intervention group being 83% and 150% higher.
Sources:
Ngandu T, Lehtisalo J, Solomon A, Levälahti E, Ahtiluoto S, Antikainen R, et al. A 2 year multi-domain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomized controlled trial. The Lancet. 2015;: p. 2255-2263.
Dementia prevention, intervention, and care: The Lancet, 2017.
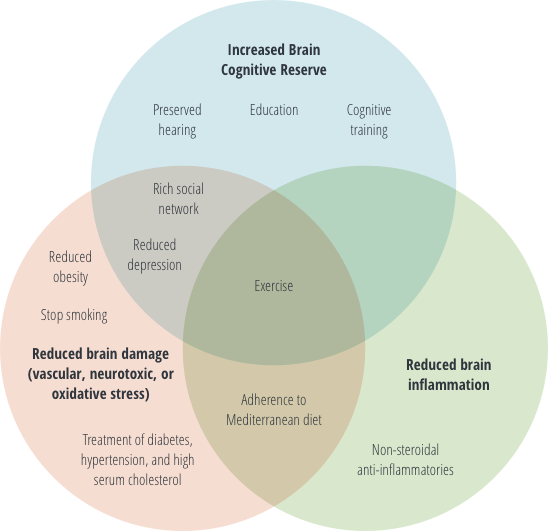
A 2017 publication titled, “Dementia prevention, intervention, and care,” concluded that one-third of dementia cases might be preventable if risk factors are addressed early on. These risk factors include: cardiovascular disease, cerebrovascular disease, metabolic factors, diet, education, and lifestyle.
It is likely that just one cause alone does not lead to dementia or Alzheimer’s, but instead it is the aggregation of multiple risk factors that ultimately lead to the disease. Since one cause does not lead to dementia, one treatment also does not resolve the symptoms or the disease. Instead, a combination of interventions, from pharmaceuticals to lifestyle changes, are needed.
The paper goes on to state the potential intervention window to delay onset of dementia is during the mild cognitive impairment stage. Since the risk factors vary per person, this stage “provides an opportunity for more targeted interventions.”
Sources:
Livingston G, Sommerlad A, Orgeta V, Costafreda SG, Huntley J, Ames D, et al. Dementia prevention, intervention, and care. The Lancet, 2017.